Q & A about safety features on the packaging of medicinal products
Change history: Changed January 16, 2026 according to updated classification guideline.
The European Commission has laid down rules for safety features on the packaging of medicinal products (see Commission Delegated Regulation (EU) 2016/161). The rules entered into force on 9 February 2019 and the purpose was to prevent that falsified medicines enter the legal supply chain for medicinal products. The new requirements for safety features on the packaging of medicinal products and a common repository system will make it possible to identify and verify the authenticity of the medicinal products covered by the rules.
In addition to the below questions and answers, we recommend that you read the guidelines published by the EMA and the HMA (see section 10 below).
The new safety features
1. What do the safety features consist of?
The regulation on safety features (2016/161 of 2 October 2015) were to be applied 9 February 2019. See the regulation. Pursuant to the regulation, certain medicinal products must bear safety features allowing the verification of whether the packaging of a medicinal product has been tampered with, and allowing the identification and authentication of the medicinal products. The safety features consist of a unique identifier/UI and an anti-tampering device/ATD. Both the unique identifier and the anti-tampering device must appear from the outer packaging or the immediate packaging if the medicinal product has no outer packaging.
The unique identifier must be encoded in a two-dimensional barcode and must at least contain:
- The product code allowing the identification of the name, the common name, the pharmaceutical form, the strength and the pack size.
- The serial number, which is a numeric or alphanumeric sequence (both numbers and letters) of a maximum of 20 characters.
- The batch number
- Expiry date
- A national reimbursement number (not relevant to medicinal products in Denmark)
This information must be encoded in the two-dimensional barcode. See Article 4. According to Article 5, manufacturers of medicinal products must print the two-dimensional barcode on the packaging. Thus, a stick-on label attached to the two-dimensional barcode cannot be used. However, in exceptional cases, it may be accepted to place the two-dimensional barcode using a stick-on label if there is no legal and/or technical alternative, e.g. due to the protection of trade mark rights or if it concerns glass/plastic packaging with no outer packaging. In such cases, the label on which the unique identifier is printed must merge with the packaging, i.e. it must not be possible to tamper with the label, and it should not be possible to remove the label without damaging the packaging or the label or without leaving any visible signs. In addition, the label on which the unique identifier is printed should be placed by the manufacturer in compliance with GMP. Regardless of this exception, it is never permitted to place the unique identifier by means of labels if this interferes with the readability. Finally, the unique identifier must not be printed on a label to be placed on an existing label as this may cause confusion and look as if it has been tampered with.
The product code, the serial number (and the national reimbursement number, if any) should be printed on the packaging in human-readable format. These requirements do not apply if the sum of the longest dimensions of the packaging equals or is less than 10 centimetres. Where the dimensions of the packaging allow it, the human-readable features must be adjacent to the two-dimensional barcode. See Article 7. It is only the product code and the serial number that must be in a human-readable format next to the two-dimensional barcode. This is not necessary for the batch number and expiry date, although they must still appear on the labelling, cf. the executive order on labelling.
The product code and the serial number must be printed on the same surface, i.e. not on different sides of the packaging.
The abbreviations PC, SN, Lot, EXP, NN do not necessarily have to be placed next to the respective human-readable data elements (product code, serial number, batch number, expiry date and the national reimbursement number, if any) or on the same line. The abbreviations can be placed anywhere, as long as it is possible to clearly identify the human-readable data elements.
The actual product code and serial number must be placed on the same surface to facilitate the manual deactivation of the unique identifier. The other data elements, i.e. batch number, expiry date and national reimbursement number, if any, must as far as possible be placed on the same surface as the product code and the serial number. If the packaging dimensions do not allow this, it is acceptable to place the other data elements as close to the product code and serial number as possible, e.g. on adjacent sides.
2. Do the new requirements for safety features replace the usual requirements for labelling etc.?
No. The requirements for safety features introduced by the regulation on safety features apply in addition to the usual requirements for labelling etc. Please note that the pharmaceutical manufacturer is responsible for ensuring that the medicinal products covered by the requirements bear the safety features. The marketing authorisation holder continues to be responsible for the medicinal product and for ensuring that the labelling etc. of the medicinal product meets the rules applicable from time to time. Please also be aware that any text elements on the labelling must be in Danish, cf. the executive order on labelling.
The unique identifier
3. Which medicinal products are covered by the regulation and will the Danish Medicines Agency extend the scope of application of the unique identifier to include all prescription-only medicinal products and all reimbursable medicinal products?
The regulation and the requirement for safety features apply to prescription-only medicinal products, unless they are included in the list set out in Annex I to the regulation. The regulation also applies to medicinal products not subject to prescription included in the list set out in Annex II to the regulation. Finally, the regulation applies to medicinal products to which the member states have extended the scope of application of the unique identifier or of the anti-tampering device. See Article 2. At present, we are not planning to extend the scope of application of the unique identifier, but we have decided to extend the scope of application for the anti-tampering device. Please see our reply to question 6.
4. Will the Danish Medicines Agency increase the contents of the unique identifier to include a national reimbursement number or other national number?
At present, we have no plans of demanding that a national reimbursement number or other number (including the item number) forms part of the unique identifier. However, we believe that all parties involved would prefer that the item number is contained in the identifier. It should be noted that the applicable rules on requirements for labelling apply in addition to the new requirements introduced by the regulation.
5. Will the two-dimensional barcode replace the existing EAN barcode?
Yes.
Please see the answer to question 7.
Anti-tampering device
Anti-tampering device
6. Will the Danish Medicines Agency extend the scope of application of the anti-tampering device to include all medicinal products, and what are the requirements for an anti-tampering device?
Yes. The Danish Medicines Agency has decided to extend the scope of application to include all medicinal products, but in a way that application is voluntary. Pharmaceutical manufacturers can choose to place an anti-tampering device on the packaging of any medicinal product, including medicinal products not subject to prescription and prescription-only medicinal products and the categories of medicinal products listed in Annex I of the regulation. This requires, however, that the pharmaceutical manufacturer based on a risk assessment has concluded in advance that the anti-tampering device will provide increased protection against falsification of the medicinal product. A decision to use an anti-tampering device is not subject to prior authorisation by the Danish Medicines Agency; nor is a notification to the Danish Medicines Agency required.
An anti-tampering device is to enable the verification of whether the packaging has been opened. An anti-tampering device is adequate if the label/gluing cannot be tampered with without leaving signs revealing that the packaging has been opened. Reference is made to the Standard EN ISO 21976:2020 “Packaging – Tamper verification features for medicinal product packaging”.
If an anti-tampering device in the form of a transparent sticker covers part of the text on the pack, the text might be damaged when opening the pack and removing the sticker. This would not conform to the labelling requirements because section 3 of the executive order on labelling provides that the labelling must be indelible. If the text is damaged on removal of the sticker, it is our opinion that the text is not indelible throughout the period of use.
On the other hand, it would be accepted to place an anti-tampering device in the form of a transparent sticker that is placed on the readable elements in the form of the product code, serial number and any national reimbursement number and/or the two-dimensional barcode, meaning that the human-readable elements and/or the two-dimensional code would be damaged or become unreadable when the pack is opened. The reason is that the mentioned readable elements and the two-dimensional barcode have served their purpose once the medicine pack has been deactivated from the database and dispensed to the patient. The other readable text elements on the medicine pack should still be indelible, cf. section 3 of the executive order on labelling.
GTIN and NTIN
7. At present, companies have major problems as to whether they should use GTIN or NTIN, including the problem that the item number cannot form part of the two-dimensional barcode when we do not share all packaging parts of the pack?
It involves in the rules that each medicinal product must bear a two-dimensional barcode containing the product code, serial number, batch number and expiry date. Consequently, many manufacturers are considering a change from NTIN to GTIN, which may pose some challenges in the supply chain, because the present systems can only handle one product line per product. In the transition period, until the systems of wholesalers, pharmacies and hospital pharmacies can handle several product lines, it is acceptable that products bear an EAN-13 barcode with an NTIN and a two-dimensional barcode with a GTIN.
It is not a regulatory activity if a company changes from NTIN to GTIN, and the Danish Medicines Agency does not record information on barcodes. We refer to this information from the Danish Medicines Verification Organisation (DMVO) and advise you to contact DMVO if you have questions about the material.
8. If a company changes from NTIN to GTIN, will packs with NTIN on the market be returned to the company, because wholesalers and pharmacies do not currently have systems that can handle the presence of multiple barcodes for the same item number? The Danish Medicines Agency needs to accept a transition period so that systems suppliers can be informed, before 9 February 2019 when the new rules of the regulation take effect, that they should be able to handle multiple barcodes for the same item number.
The Danish Medicines Agency finds that these matters should be solved in collaboration between the industry and the system supplier. We kindly refer to the Danish Medicines Verification Organisation, www.dmvo.dk.
Regulatory implementation
9. How should the anti-tampering device be implemented?
Where the anti-tampering device is placed on the outer packaging and the readability is not affected, and neither the immediate packaging (container), nor the closure system is affected, and no changes are to be made to the summary of product characteristics or the documents forming the basis for a marketing authorisation, a variation application or other regulatory activity should not be submitted.
We refer to the above implementation plans from the EMA and CMDh, which state as follows: ”implementation of the ATD is not expected to impact the product information. However, when the ATD is placed on the immediate packaging because there is no outer packaging, certain section(s) of the marketing authorization dossier may be impacted. (…) Concerning the ATD, in the case of medicinal products where the ATD is placed on the immediate packaging because there is no outer packaging and the ATD affects the container and its closure system(s), applicants are required to submit the appropriate variations to include the information on the ATD and how the ATD affects the container and its closure system(s). (…) If the ATD does not affect the container and its closure system, or is placed on the outer packaging, no regulatory procedure is necessary. However, if the addition of the ATD has an impact on the readability of the packaging information, MAHs are requested to submit a Notification pursuant to article 61(3) of Directive 2001/83/EC to register the change”.
10. How should the two-dimensional barcode be implemented?
The implementation of the two-dimensional barcode requires an updating of the QRD template (Annex IIIA, sections 17 and 18). In the CMDh annotated QRD template, you can read more about what to indicate under sections 17 and 18 to obtain authorisation from the Danish Medicines Agency.
An update in line with the QRD template is generally classified as a type IB variation under category C.z. See the CMDh Q&A about Variations nr. 2.11.b. However, an update solely in line with sections 17 and 18 of the QRD template is classified as an article 61.3 notification.
As regards nationally authorised medicinal products, the Danish Medicines Agency follows the CMDh recommendations. The CMDh recommends that the update in line with sections 17 and 18 of the QRD template takes place in connection with the submission of another regulatory activity affecting the product information (type IA/IB/II variation or renewal). The labelling must be updated in line with sections 17 and 18 of the QRD template before the rules governing safety features become effective on 9 February 2019. If it is not possible to make the update in connection with another regulatory activity affecting the product information, an article 61.3 notification should be submitted.
Please note that the Danish Medicines Agency does not request that the updating of the labelling in line with sections 17 and 18 of the QRD template has been approved before the two-dimensional barcode is placed on the outer packaging. As long as the updating of the QRD template is made before the rules enter into force on 9 February 2019, it is possible to add the two-dimensional barcode before sections 17 and 18 of the QRD template have been approved. Please note that if you add the two-dimensional barcode before you apply for approval of the updating in line with the QRD template, the updating must be included in the first-coming regulatory activity affecting the product information, alternatively you must apply for an article 61.3 notification as described above.
See the implementation plans of the CMDh and the EMA:
11. Which requirements apply to the submission of a variation application for the implementation of the unique identifier? If the application is submitted well in advance, e.g. together with another variation about updates of the packaging material, the deadline for implementation is usually one year. In that case, should the unique identifier also be implemented within one year or is it possible to select another time for the implementation?
According to the CMDh and EMA implementation plans, an approval of a variation related to the updated QRD template (sections 17 and 18 of the labelling) is not the same as an implementation – regardless of the deadline for implementation approved for the remaining part of the variation. This applies to cases where updates in line with the QRD template only form part of the overall variation.
Note that the rules only apply to packs of medicinal products released for sale or distribution etc. after 9 February 2019, see the transitional measures laid down in article 48 of the regulation.
We expect the companies to update their common texts on an ongoing basis, see sections 17 and 18 of the QRD template. See the answer to question 10.
12. In the opinion of the Danish Medicines Agency, can batches without two-dimensional barcodes etc. thus not be released after the implementation deadline on 9 February 2019? Or does the Danish Medicines Agency define implementation in a different way than the other countries (e.g. supply to a wholesaler as for other variations)?
According to article 48 of the regulation on safety measures, medicinal products that have been released for sale or distribution without the safety features in a member state before the date on which this regulation becomes applicable in that member state, and are not repackaged or relabelled thereafter, may be placed on the market, distributed and supplied to the public in that member state until their expiry date. Moreover, it appears from recital 43 that in order to avoid disruptions in the supply of medicinal products, transitional measures are necessary for medicinal products which have been released for sale or distribution without the safety features before 9 February 2019.
In the opinion of the Danish Medicines Agency, this means that medicinal products which are released before 9 February 2019 without the safety measures and are not repackaged or relabelled thereafter can form part of the entire subsequent distribution, including by wholesalers.
13. What will happen to the national authorisation procedure for the labelling document? Will the Danish Medicines Agency assess and approve the text document?
At present, there are no planned changes to the authorisation procedure. See the CMDh implementation plan above.
14. Today, national marketing authorisations do not have a labelling document. If there is such document, it may not necessarily be updated. What will the future procedure be like for approval of the labelling document for national marketing authorisations?
See the answer to question 13.
15. If there is no need for submitting a variation within the time frame, the change must be submitted as a notification at “an early stage”. What is at ”an early stage” – deadline for the submission of a notification?
Generally, companies can expect that the Danish Medicines Agency meets the deadlines applying to our assessment of variations, but if we suddenly receive a very large number of variation applications, this may increase assessment times. Consequently, we encourage you not to wait too long before you submit the required variations.
16. Is it acceptable to implement the safety features when the location and the NMVO are ready, and thus deviate from the usual requirements for the implementation of text changes?
If the rules on variations are complied with, it is acceptable to implement the safety features before the rules become effective on 9 February 2019. In that case, the two-dimensional barcodes should be uploaded as soon as possible.
17. What does the Danish Medicines Agency expect the marketing authorisation holder to indicate under sections 17 and 18, see the QRD text template, to obtain approval from the Danish Medicines Agency?
See the CMDh’s annotated QRD template:
See the answer to question 10.
18. How should a variation be applied for in order to include the safety features in sections 17 and 18 in the QRD v10?
As regards medicinal products authorised under the purely national procedure, we will follow the CMDh implementation plan. This means that we recommend you to submit the variation together with another variation, and if no regulatory procedure occurs within the stated time frame, then you are requested to submit a notification pursuant to article 61.3.
See the answer to question 10.
19. Which documents should be attached to the application?
We expect you to submit either a variation application form, alternatively the 61.3 notification form (see the CMDh’s website).
The QRD template should also be used and submitted for medicinal products authorised under the purely national procedure. See the answer to question 10.
Any other documentation may be required if you apply for other variations at the same time.
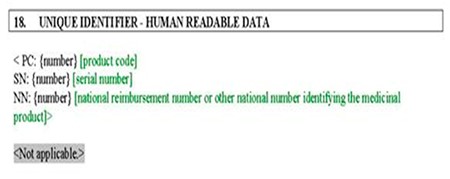
20. The QRD template states for outer packaging, section 18: Unique identifier – human readable data. If relevant for product concerned, should ”PC, SN, NN” or ”product code, serial number, national or other national number identifying the medicinal product” be indicated?
Under section 18, please write the text printed in black, that is ”Not applicable” or ”PC: {number} SN: etc.”. The text printed in green is meant as a help to explain which information is included in the various codes. For purely national marketing authorisations, please state ”Not applicable” under ”NN”. Please follow the same order as in the QRD template. The batch number and expiry date must thus not be placed, for example, in between the product code and the serial number. Otherwise, the rules for placing the batch number and the expiry date are unchanged, i.e. there is no requirement for placing the batch number or expiry date first.
Please also note that the abbreviations ”PC” (and thus not numbers or GTIN, etc.), ”SN” and ”NN” must be used.
In its Q&A document, the Commission provides that the manufacturers should be able to choose the order of both the data elements and the unique identifier regarding the human-readable data. This means that the order of the QRD template or the order laid down in the regulation’s article 4(b) and article 7(1) are not binding on the manufacturers. This approach has been chosen to exhibit flexibility.
21. We can update the QRD template in connection with another updating of the product information, but can we also submit a grouped application and have the updates approved for all relevant products at the same time?
It is not possible to submit a grouped application, since only IA notifications can be grouped across products. This variation is not classified as an IA variation, see the CMDh implementation plan (section 8).
We recommend that you make the change in connection with another regulatory activity, see the CMDh implementation plan. If no regulatory activity occurs within the time frame and no later than 9 February 2019, a notification pursuant to article 61.3 must be submitted. See the answer to question 10.
Item number
22. Both GTIN and NTIN are accepted and the requirement as to item number is maintained, but NTIN does not necessarily comply with the GS1 standards.
Will the Danish Medicines Agency support initiatives to introduce systems that can handle several EAN codes related to an item number or initiatives to an amendment procedure for EAN, perhaps ”set up” solutions as those introduced in Sweden or Finland?
What does the Danish Medicines Agency recommend as regards a continued link from the product code to the item number if the product code is changed?
The item number must still appear from the packaging in human-readable format, and if the item number is printed adjacent to the two-dimensional barcode in human-readable format, it does not need to be printed elsewhere on the packaging.
At present, we have no plans of demanding that a national reimbursement number or other number (including the item number) forms part of the two-dimensional barcode. However, the product code may be encoded in the two-dimensional barcode. See, for example, consideration 13 according to which the two-dimensional barcode may store more information than the data elements of the unique identifier as it should be possible to use that residual storage capacity to carry further information and avoid the placing of additional barcodes.
Pursuant to article 5 of the regulation, unique identifiers with a coding scheme, which conforms to the ISO/IEC 15418:2009, are presumed to fulfil the requirements. If NTIN does not comply with the standard, it cannot be used. We recommend that you contact the DMVO for more information, see www.dmvo.dk
The existing challenges regarding item numbers and Nordic packs are not affected by the requirements to implement safety features, and these challenges should be solved between the affected parties, however, in our opinion the system should preferably be able to handle several EAN codes.
23. Chapter 4 of the guideline to the executive order on labelling etc. of medicinal products specifies that the medicinal product’s name, strength, form, pack size and item number should be placed horizontally in the same visual field. Would it be acceptable to let the item number form part of the two-dimensional barcode printed on the “back of the pack” and not in the same visual field as the name, strength, form and pack size?
The item number can be placed in human-readable format on the back of the pack adjacent to the two-dimensional barcode.
Dispensing from pharmacies and hospital pharmacies
24. Can pharmacies dispense medicinal products with safety features if the repositories system is unavailable due to temporary IT problems?
Yes, on condition that verification of the authenticity and decommissioning is carried out as soon as the repositories system is available and that the integrity of the anti-tampering device is verified before the product is supplied to the public. Moreover, in case of suspected falsification of medicinal products, the recipients must be informed immediately to prevent that the medicinal product is used and to ensure that the medicinal product is returned to the pharmacy.
25. What should a pharmacy/hospital pharmacy do if a medicinal product cannot be verified in the repositories system?
If there is reason to believe that the packaging of the medicinal product has been tampered with or the verification of the safety features of the medicinal product indicates that the product may not be authentic, the medicinal product must not be supplied to the public by the pharmacy/hospital. Read guiding text for additional information: Safety features - handling of alerts
26. Can a hospital pharmacy reverse the status of a decommissioned unique identifier of a medicinal product supplied to a hospital ward that has subsequently returned the medicinal product to the hospital pharmacy?
Yes. Manufacturers, wholesalers and persons authorised or entitled to supply medicinal products to the public, including hospital pharmacies, may only revert the status of a decommissioned unique identifier to an active status if the following conditions are fulfilled:
a) The person performing the reverting operation is covered by the same authorisation or entitlement and operates in the same premises as the person that decommissioned the unique identifier.
b) The reverting of the status takes place not more than 10 days after the unique identifier was decommissioned.
c) The pack of medicinal product has not expired.
d) The pack of medicinal product has not been registered in the repositories system as recalled, withdrawn, intended for destruction or stolen and the person performing the reverting operation does not have knowledge that the pack is stolen.
e) The medicinal product has not been supplied to the public.
Medicinal products bearing a unique identifier which cannot be reverted to an active status because the conditions set out in paragraph 1 are not fulfilled must not be returned to saleable stock.
See article 13 of the regulation.
27. Can the pharmacy dispense a pack of medicinal product to a customer if the anti-tampering device has been tampered with but the pack was not dispensed, e.g. because the customer did not want the medicinal product?
The regulation does not prevent such dispensing, but if the pack of medicinal product has also been decommissioned in the repositories system, the dispensing must take place in accordance with article 13 of the regulation. This implies that the pharmacy must guarantee that the pack of medicinal product was opened by the pharmacy. See the answer to question 23.
Parallel import
28. Would it be against the regulation if a parallel importer replaces the anti-tampering device with another device?
The Danish Medicines Agency can refer to the judgements in the following cases:
- The Merck-judgement, C-224/20: CURIA - Resultatliste (europa.eu)
- The Bayer-judgement, C-204/20: EUR-Lex - 62020CJ0204 - EN - EUR-Lex (europa.eu)
- The Novartis-judgement, C-147/20: EUR-Lex - 62020CJ0147 - EN - EUR-Lex (europa.eu)
Please also see The Commissions Q & A (the answer to question 1.20: Safety features for medicinal products for human use
29. Should parallel importers, just like other marketing authorisation holders, submit notifications/variations in connection with the implementation of the safety features?
Yes, parallel importers should, just like other marketing authorisation holders, submit notifications/variations in connection with the implementation of the safety features. Please use the QRD template for this purpose.
Over-the-counter medicines
30. Can over-the-counter medicines be labelled with a two-dimensional barcode as long as it is not a safety feature, i.e. contains a product code in combination with a serial number?
Yes. In the opinion of the Danish Medicines Agency, the content of the code (UI etc.) constitutes the safety feature. Consequently, over-the-counter medicines can be labelled with a two-dimensional barcode as long as it does not constitute a safety feature, i.e. contains a product code in combination with a serial number.
Miscellaneous
31. The legislation stipulates that certain types of customers should be treated in a special way in relation to the decommissioning of the unique identifier. The list includes prisons, schools, hospices and many other institutions. Can the Danish Medicines Agency prepare a similar list based on Danish conditions which outlines the institutions that should be treated in a special way?
The list contained in the regulation is exhaustive, and we have no knowledge of institutions in Denmark that should be covered by the list.
32. What are the requirements in cases where a medicinal product in one pack and a medical device in another pack are wrapped by cellophane?
Only the pack of medicinal product is considered as the outer packaging that should bear the safety features. According to Article 5, manufacturers of medicinal products must print the barcode on the packaging.
33. How do we apply for an exemption from the obligation to verify the safety features (the white list)?
The final lists adopted by the European Commission are set out in Annexes I and II to the regulation on safety features.
Based on recommendations from the member states, the European Commission decides which medicinal products should be included on the lists, taking into account the five criteria. Consequently, companies cannot apply for exemption from the list.
See article 54a of the Directive on medicinal products for human use
See also articles 46 and 47 of the regulation on safety features in the link above.
The lists apply from 9 February 2019 when the regulation enters into force. Changes to the present lists – additions or removals of medicinal products from the lists – require an amendment of the regulation to be adopted by the European Commission.
The European Commission can decide that a medicinal product should not bear the safety features (”white list” which means that the medicinal product will be included in Annex I to the regulation on safety features) but the risks of falsification must have been assessed. The assessment must, as a minimum, take into account, the five criteria set out in articles 54a(b) (i)-(v) of the directive.
The Danish Medicines Agency has not yet established any practice on how and to what extent we will recommend that medicinal products are included on the ”white list”, see article 46(2) of the regulation on safety features. The first step would be a request from the marketing authorisation holder, including arguments related to the specified criteria as well as other matters that the MAH believes are of importance to an assessment of the risk of falsification.
Even if the Danish Medicines Agency decides to report a medicinal product to the European Commission on that basis, it should be noted that the European Commission makes the final decision and that this decision will apply throughout the EU. Moreover, such a process will normally take at least two years.
The Commission has provided guidelines for the Member States in connection with the national assessment of requests for admission to the white lists and the five criteria established in the directive. The Commission has stated that a medicinal product is required to fulfil the five criteria in a majority of Member States before being admitted to the lists.
The price and sales volume of the medicinal product: The price criterion must reflect the costs of manufacturing falsified medicinal products as well as the likely sales price to establish when falsification becomes economically unattractive. The costs of manufacturing falsified medicinal products are often very low, sometimes even close to zero. Therefore, medicinal products with a pharmacy price above EUR 5 or a wholesale price above EUR 3 or a manufacturer’s price above EUR 2.7 are likely to generate considerable profits for those falsifying medicinal products. Furthermore, the risk of falsification of medicinal products marketed in very low volumes is smaller because of the economic aspect.
The number and frequency of previous cases of falsified medicinal products being reported within the Union and in third countries and the evolution of the number and frequency of such cases to date: The number of cases of falsified medicinal products in the legal supply chain should be taken into account when the cases are reported by the EU authorities via official channels, by third countries through the EU’s rapid alert system or by third countries with which the EU has mutual recognition agreements on standards via official channels.
The specific characteristics of the medicinal products concerned: Medicinal products that could have specific characteristics that increase the risk of falsification. This is the case for medicinal products that have been falsified before, such as medicinal products for erectile dysfunction, weight loss and eating disorders, inhibitors and stimulants of the central nervous system and anabolic steroids.
The severity of the conditions intended to be treated: Usually, falsified medicinal products do not have the same effect as the original product. For example, the active substance may not be present in the falsified version or it may be present in a higher or lower concentration than the original product. It is particularly important to prevent the falsification of essential and life-prolonging medicinal products because it may have severe or fatal consequences for those patients who do not receive the right treatment or are not diagnosed in time. Essential or life-prolonging medicinal products should be assessed on the basis of both the nature of the life-threatening disease to be treated or diagnosed and the medicinal product’s importance in treatment or diagnosis of the disease in question. A life-threatening disease is defined as a disease or condition where the likelihood of dying in the short-term is high if the patient discontinues effective treatment or is misdiagnosed because of a falsified medicinal product. Life-prolonging medicinal products may include, but are not limited to, medicinal products with indications for treatment or diagnosis of the following: 1) Cancer, 2) Life-threatening cardiovascular diseases (certain cardiac arrhythmias, heart attacks, strokes), 3) Diabetes, 4) HIV, 5) Certain rare diseases, 6) Life-threatening respiratory diseases (e.g. COPD, asthma, tuberculosis, pneumonia) and 7) Life-threatening neurological diseases (e.g. epilepsy, amyotrophic lateral sclerosis).
Other potential risks to public health: Other potential risks to public health caused by falsification of specific medicinal products should also be considered in the risk assessment, e.g. anti-infective medicinal products (antibiotics, antivirals, antifungal and antiparasitic drugs), as the falsification of antibiotics and other antiinfective agents may increase antimicrobial resistance, or vaccines since the falsification of vaccines could prevent the effective response in case of pandemics. Consequently, the falsification of the medicinal product should not constitute a significant risk to public health.
34. Do the new rules cover medicinal products not on the market or medicinal products dispensed according to a compassionate use permit?
The Danish Medicines Agency considers the regulation on safety features to cover authorised medicinal products released for sale or distribution. This means that marketed medicines which are covered by the new requirements for the placing of safety features but are not on the market do not necessarily have to be added the safety features. However, you should be aware that the placing of safety features on such medicinal products is required once the medicines are released for sale or distribution.
The requirement that the regulation on safety measures covers authorised medicinal products also means that medicinal products that are not marketed in Denmark and thus not released for sale of distribution in Denmark are not covered by the new requirements of the regulation. Be aware, however, that medicinal products authorised within the EU and released for sale or distribution in the EU are covered by the requirements, and safety features, etc. must therefore be placed on them in the country in which the medicinal products are marketed.
Thus, it is our opinion that a medicinal product not authorised in the EU, but authorised in for example a non-EU country, is exempt from the rules when dispensed to patients according to a compassionate use permit obtained by a doctor.
Correspondingly, magistral formulas (medicines prepared for a specific patient) fall outside the new regulation rules because of the fact that these are not authorised medicinal products.
35. Will the new rules imply that the Danish Medicines Agency will be approving the labelling of medicinal products?
No, we will not change our current practice of approving the labelling of medicinal products as a result of the new rules.
36. Where can I find additional information?
See the Commission Delegated Regulation (EU) 2016/161 on safety features
See The Commission’s Q&A on safety features. Click on "Questions and Answers document".
For more information about the DMVO, see www.dmvo.dk